Interview with: Dr Laura Indolfi from PanTher Therapeutics about localized chemotherapy.
Dr Laura Indolfi speaks to Materials Today about her recent paper published in the journal Biomaterials. Follow the link below, to listen to the interview, or right click to download. Click here to read the article, A tunable delivery platform to provide local chemotherapy for pancreatic ductal adenocarcinoma.
Listen nowStewart Bland: I’d like to ask if you can start by introducing yourself, PanTher, and telling us about your background?
Laura Indolfi: Yes, so I am Laura Indolfi. I’m the founder and CEO of PanTher Therapeutics, which is a northerly state biotech start up based in Boston, Massachusetts, and we have revolutionised the way we deliver chemotherapeutic agents directly at the tumour site. I am a biomedical engineer. My training was in Italy, and then I moved to Boston to do my post doc at the Massachusetts Institute of Technology, and during my tenure there, we started this project in collaboration with oncologists at the Massachusetts General Hospital, to find a new way to treat cancer, and pancreatic cancer was one of our leading indications.
Stewart Bland: In your study published in the journal, Biomaterials, you reported on a new platform to provide local chemotherapy for pancreatic ductal adenocarcinoma. Before we discuss the development, can you tell us more about this condition?
Laura Indolfi: Yes, sure, so pancreatic cancer is a raising type of cancer. It has been established as the third leading cause of cancer deaths worldwide, just after lung cancer and colon cancer, and unfortunately, in the last 40 years, the survival rates of those patients hasn’t changed, so the diagnosis and the survival numbers for those tumour types are almost equal. Every year the same number of patients get diagnosed than the ones that died, so the treatments that there is right now on the table are definitely not effective. Because of the anatomical position of the pancreas, the tumour can spread, so it can enter into many vital organs that surround the pancreas, like the stomach, the liver, the coeliac nerves, and make the life of the patient very painful. So not only is it a tumour that’s spread very easily, but it also spreads in very vital organs, making the quality of life and prognosis very poor for those patients, so that’s a little bit of the general description of pancreatic cancer. Also it’s a very silent disease, so it gets diagnosed when it’s usually too big to be removed, leaving very few alternatives for those patients, other than the standard treatment, which is the injection of drugs into the bloodstream, with the aim that, in some magical way, going around throughout all of the body, they will find their avenue to go into the tumour mass, and be effective.
Stewart Bland: I think you touched on this in that answer, but could you say a little bit more about why it’s important to develop a new treatment for this particular condition?
Laura Indolfi: Yes, I touched a little bit, saying that it’s spread into other organs, but also I also said that the only treatment currently available is the systemic injection, so being able to deliver the drug into the bloodstream to reach the tumour mass. Unfortunately, for this particular condition, the tumours don’t have a lot of vessels within it, so if we think of the bloodstream as a highway that carries the drug to the tumour, we have no access to this highway into the tumour itself, so the drug goes everywhere else in the body, but very little will actually reach the tumour site. So we need a new treatment that can provide a better delivery of the weapon (the tumour therapeutic agent) directly at the tumour site to be effective. A lot of drugs have been designed and developed by a pharma company that can be very useful for pancreatic cancer, and also for many other types of solid tumours, but the inability of the drug itself to reach the tumour mass is what has been hindering the success of those drugs, so that’s where we kind of came along, and why we need this; it is important to deliver new localised treatment for pancreatic cancer, and many other solid tumours as well.
Stewart Bland: Now, can you tell us about the delivery device that you’ve developed, and what does it do, and how does it work?
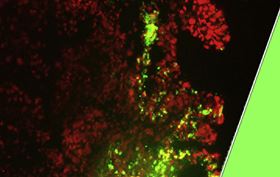
Laura Indolfi: The interesting thing in our approach is that we have combined an engineer like myself, with the oncologists that treat those patients, and we have been very creative in trying to combine the two different knowledge bases to provide a solution for these patients, and what we have come up with is; we designed a platform that can be placed in direct contact with the tumour, and so is some sort of Trojan horse - so it’s a material which is very inert with the body, that can be placed in direct contact with the tumour, and over time the material itself will dissolve, and the drug will be released directly into the tumour mass, to increase therapeutic efficacy, and to decrease the systemic exposure, so the exposure of other parts of the body to the drug, that it’s usually the source of complications and side-effects. We designed our first product to be like a Band-Aid, as a patch, that can be placed, minimally invasive, in direct contact with the tumour, so the patients don’t need to undergo surgery. They can just have a laparoscopic procedure, where this patch can be folded in a cigar shape, and can then be unfolded on the other side of the catheter, to be wrapped like a blanket on top of the tumour, and this will serve as a two-fold weapon, on one side being able to place a solid blanket on top of the tumour, will help in preventing the continuous spreading of the tumour into other organs, so in case, where the tumour, it’s very confined, and has not yet invaded other organs, the ability to place this blanket will prevent the metastasis into the nearby organs, like the liver, the stomach, and at the same time, as the blanket will dissolve, the drug will be delivered in direct contact with the tumour, allowing for a better response to treatment that can shrink the tumour to a side where the surgeon feels confident that it can be removed.
Stewart Bland: So can you tell us a little bit about the testing of the device, and the success?
Laura Indolfi: So we have created these animal models, where we have implanted human tumours, human pancreatic tumours, into the pancreas of mice, and then once the microenvironment was recapitulated, so we have tumours into these mice in the pancreas, we either treated those animals with the standard of care of injecting the drug into the bloodstream for four weeks, or we placed it on top of the tumour, our mouse-sized prototype of the device, that was providing for a sustained release over the same time period of four weeks of the same drugs at the same concentration, so basically we wanted to test if the delivery method of the same amount of drugs, of the same drug, was going to have any effect of treatment, and in very good news and very surprisingly, we found that we were able to improve the response of treatment of twelve times, so the same amount of drugs, of the same drug, in the same animal model, but just delivered differently, allowed us to have a huge increase in the response to treatment, where the tumour has shrunk in dimension. They become very necrotic, so they were dead cells that could be easily removed in case of surgery, and we were also able to extend the survival rate of those animals, so the group that received the drug ivs, so into the bloodstream, they became sick very fast, and they died over a very short period of time, while the group that received our localised implant were able to live longer. Actually we had 100% to zero survival rate, so when all of the animals into the control group died, we had still all the animals alive in the localised delivery, that it’s a huge response for that tumour type, because the patients in the clinic, they have a very short life expectancy, so if we had the localised delivery, we can improve and prolong their survival rate, we will be affecting the life of thousands of patients worldwide, and another thing that we were not really expecting, but it’s going to be a very huge benefit for patients, is that we also showed that the ability of giving the drug locally at the primary tumour site affected the ability of the tumour to spread and metastasize also in a very distant part of the body, so when the animal group was treated with the drug injected in the bloodstream, they develop lung metastasis, while when we used our device for doing a localised delivery of the drug, because we were able to kill the primary source of the tumour, so the primary mass, there was no lung metastasis at the end of the study, and that’s because we are basically killing the primary source of the cells, and then they go around in the body and find another place, where to create their home, so this is something that will have a huge impact into the clinic, if we think of patients, that they can get diagnosed before the tumour has spread into other organs, they can have this blanket placed on top, shrunk to a size where the primary tumour can be removed, and also allow for prevention of the spreading into other organs, that then can cause a recurrence of the disease, or some more complication of the treatment, so all in all we had very good data that allowed us to be very enthusiastic about the possibility of bringing this treatment into the clinic for a disease that currently has a very poor outcome and no alternatives whatsoever.
Stewart Bland: So what's next for the project?
Laura Indolfi: So since then, we have spin out the company, PanTher Therapeutics, into our time at the MIT and MGH, because we want to bring this technology into the clinic. We are working very closely with the FDA to obtain all of the approval and the certification to start testing this treatment into the humans, so we are finalising a large animal model testing to be sure that the procedure of implantation in clinical settings, it’s safe and it’s reproducible, and if everything goes as we are planning in the next twelve months, we may be able to obtain FDA approval to start first-in-man clinical trials, and we can begin the testing into the patients. At the same time, we are also expanding the pipeline, so as I was mentioning at the beginning, all of this limitation of treating cancer, they are not only confined with pancreatic cancer, but most of the major solid tumours, colon, any type of gastrointestinal, solid tumour, they are very difficult to be reached by a surgeon, differently from what happens with breast cancer, for example, for all of this type of disease, an approach like ours, using our blanket to cover the tumour, and deliver the drug locally, can be very beneficial, so we are expanding beyond pancreatic cancer to make this treatment available for other types of disease as well, of the tumour site as well, and in parallel we are preparing a platform of agents that we can embed into this blanket, so we have chosen one drug that we have tested until now, but the beauty of this approach is that it’s a very versatile one, where we can put inside the blanket different types of drugs, even multiple drugs that can be released in a different way at different times, to provide a more comprehensive line of treatment for killing cancer, and making a new treatment solution for this disease, so we have a lot of work to go ahead, but we are very thrilled, and we are very galvanised by the early data that we have provided, so there is a lot of work to do, but we are very hopeful that we can bring a new solution for the treatment of cancer to the patients very soon.
Stewart Bland: Excellent, well that’s fantastic to hear. So finally, as always, I’d like to ask, in your opinion, what are the hot topics in materials science right now?
Laura Indolfi: I think that there is, I may be biased on that, because it’s the area where we are working on, but I really think that there is an untapped area of really providing a localised solution for delivering drugs, or for allowing regeneration of organs. Until now, medicine has been very focused on a systemic and whole body treatment for many diseases, and as material science progresses, and there is all of this combination of natural and synthetic material, or material that can recapitulate a biological clue, can sense a biological clue when inserted into the body and respond accordingly, this is a new area where materials science has a lot to bring on the table, to improve treatment in medicine, and I think that like us, many others are working in the field, we are really excited and intrigued to be at the forefront of engineering and medical science, to combine new material and old material reformulated, to have a huge impact in the development of new medical treatment in cancer and beyond.