Globally, each year millions of patients undergo clinical transplant procedures to replace damaged or diseased bone tissues. The use of the patients own bone (autograft) is well established, delivers positive clinical outcomes and is considered the gold standard. The positive result arises from ideal biocompatibility and osteogenic properties that deliver bone-forming cells to the implant site. Unfortunately, autograft procedures also suffer from two serious side effects. Firstly, the number of potential donor sites available to the surgical team is limited and secondly, donor site morbidity at the harvested site is a major concern. Because of these two side effects medical researchers have looked for alternative sources of suitable bone tissue [1]. Bone tissues can be sourced from other donors (allogenic bone grafts), but obtaining a supply of high quality medical grade bone tissue is difficult due to medical, ethical and legal concerns. The medical concerns centre on the unfavourable inflammatory response from the body's immune system and the risk of disease transmission [2]. Because of these concerns, medical research has focused on searching for innovative materials that can be formed into implants and successfully used as alternatives to natural bone grafts. Currently, the majority of implants used for load bearing orthopaedic applications are manufactured from metal alloys like cobalt-chromium, stainless steels and titanium. In spite of their attractive mechanical properties like favourable ductility, high strength and excellent fracture toughness there are several detrimental side effects resulting from the use of these metal alloys [3] ; [4]. These side effects include the release of toxic chromium, cobalt and nickel ions during mechanical wear, inflammatory responses to the ions, and stress shielding resulting from the significant differences between elastic moduli of implant and surrounding bone. The stress shielding phenomena initiates bone resorption in the vicinity of the implant and weakens the surrounding bone structure. The situation is further exacerbated by poor interfacial bonding and osteointegration taking place due to the inert nature of the metal implant [5]. Ultimately, these side effects lead to implant failure and results in costly secondary revision surgeries, increased risk of infection and produces further patient scarring.
However, biodegradable implant materials are designed to undergo complete dissolution by the end of tissue regeneration and the healing period [6]. For example, biodegradable polymers are successfully used in a variety of clinical applications that require sutures, grafting materials and fixation devices [7]. Unfortunately, polymers also have low mechanical strength and so are predominantly used in soft tissue repair and low-load bearing applications. However, recent studies have shown that magnesium has the capability to overcome many of the limitations associated with both conventional metallic implants and biodegradable polymers. The close similarity of magnesium's mechanical properties to those of bone, and its favourable biocompatibility profile make magnesium a very promising candidate for biodegradable orthopaedic implants [8]. In spite of these advantages, pure magnesium has poor corrosion resistance in chloride rich body fluids and its rapid degradation poses two fundamental problems. The first problem is the formation of subcutaneous hydrogen gas bubbles that appear soon after surgery. While the second problem results from the loss in mechanical integrity of the magnesium implant caused by the rapid corrosion process. However, magnesium's vulnerability to degradation within the body environment can also be considered an advantage if a corrosion regulating mechanism is incorporated into the design of the bio-implant. Thus, matching the degradation rate with the formation rate of new bone tissues that ultimately replaces the degrading implant is the ultimate goal of this clinical procedure [9]. One method of regulating the corrosion rate is by using an appropriate biocompatible coating. Calcium phosphate coatings are currently used on a variety of metal implants because they offer good biocompatibility and good osteoinductivity capabilities [10] ; [11].
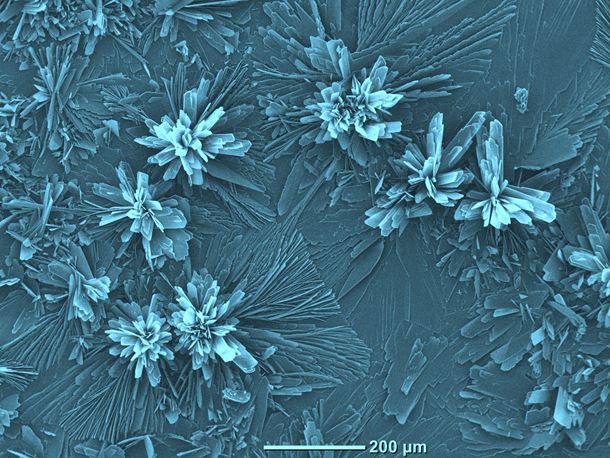
This issue's cover of Materials Today, presents a scanning electron microscopy image of flower-like Brushite [Di-calcium phosphate di-hydrate (DCPD)] crystal structures formed on the surface of a magnesium substrate by chemical immersion. The substrate was mounted on the sample holder using carbon adhesive tape. The substrate was then sputter coated with a 2 nm layer of gold to prevent charge build up using a Cressington 208HR High Resolution Sputter coater. The image was taken using a JCM-6000, NeoScope™ fitted with an energy dispersive X-ray spectroscopy function. The image was colour enhanced to highlight the ornate and beautiful flower-like crystal structures formed during 60 min of immersion. Degradation studies carried out on uncoated magnesium substrates in Ringer's solution at 37 °C were found to have a mean corrosion rate of 3.828 mm/year. While substrates coated with Brushite were found to have much lower corrosion rates that were typically around 0.100 mm/year. Thus, demonstrating that varying the coating thickness produced during chemical immersion can control the magnesium's corrosion rate [12]. Research is ongoing, designed to optimise the chemical immersion process and fine-tuning of degradation profiles for various coating types.
Further reading
[1] S. Kao, et al.
Oral. Maxillofac. Surg. Clin. North Am., 19 (2007), pp. 513–521
[2] V. Ng
Orthopaedics, 35 (2012), pp. 679–681
[3] M. Geetha, et al.
Prog. Mat. Sci., 54 (2009), pp. 397–425
[4] C. Lhotka, et al.
J. Orthopaedic Res., 21 (2003), pp. 189–195
[5] D.F. Williams
J. Mater. Sci., 22 (1987), pp. 3421–3445
[6] P. Habibovic, et al.
J. Tissue Eng. Regen. Med., 1 (2007), pp. 25–32
[7] M. Todo, et al.
Eng. Fracture Mech., 74 (2007), pp. 1872–1883
[8] G.E.J. Poinern, et al.
Am. J. Biomed. Eng., 2 (2012), pp. 218–240
[9] F. Witte, et al.
Biomaterials, 26 (2005), pp. 3557–3563
[10] S. Shadanbaz, et al.
Acta Biomater., 8 (2012), pp. 20–30
[11] G.E.J. Poinern, et al.
Scientific Rep., 4 (2014), pp. 1–9
[12] S. Brundavanam, et al.
Am. J. Biomed. Eng., 4 (2014), pp. 79–87